Please view our updated COVID-19 guidelines and visiting procedures →.
If you have ever wondered, "What happens at hospice?" or, "What to expect for hospice care?" This post will walk you through a day in the life of a hospice.

People have preconceived notions about what hospice life must be like, and it usually involves words like “depressing”, “sad”, or “painful”. Connecticut Hospice, the country’s first hospice and a pioneer in end of life care for almost fifty years, is none of those things.
If one were to walk onto the inpatient floor, very early in the morning, the first impression is one of peace and quiet. There are no beeping machines, overhead lights, or loudly speaking caregivers, that characterize so many other health care institutions. Here, they are still hours from breakfast, with family members who have slept on a cot at the bedside of a loved one roaming the halls, looking for fresh coffee on each end of the floor. Nurses and doctors are whispering morning greetings, and huddling about the patients and their conditions overnight. Everyone who is awake is soon watching another beautiful sunrise over Long Island Sound. No matter the weather, or the season, it’s always a joy to see the sun come up over the water at our 52-bed, waterfront inpatient facility.
On the other floors, home healthcare nurses and aides are picking up supplies, checking in with supervisors, and communing over whatever snacks have been left out by grateful families. Maintenance and kitchen workers are going about their days, while office workers are settling in for the morning. The pharmacy is buzzing with activity, as they calibrate dosages and adjust drugs after the night reports are in. Early birds have begun to churn out their work, while other offices await occupants.
Not everyone wears scrubs, but many do, especially if they interact with patients. Nurses and Certified Nurse Assistants each have special colors, except on Friday, when any color goes. The holidays bring a relaxation of the color rules, and a lot more red and green apparel is seen, along with reindeer headbands. In other departments, people can wear any color, though the current favorite is probably black, which is far more chic than the baggy blue handed out to staff. One such fashion plate has even had his monogrammed!


9 AM is midmorning for some, but many other people are still arriving. The official start of many homecare days is the IDT meeting. That stands for Interdisciplinary Team, which is what Medicare requires for care coordination. Our comprehensive approach to hospice and palliative care is delivered by a medically directed, nurse-coordinated, interdisciplinary team, which consists of hospice and palliative board-certified physicians, nurses and pharmacists.
Despite its being required, many professionals have come to love the IDT meetings. Much of their time is spent on the road and working alone with patients and families, so they value the camaraderie and mutual support of the IDT. Teaching also takes place, with doctors and supervisors sharing medical knowledge or regulatory updates. The meeting can last for two or two and a half hours, after which everyone rushes off to begin daily home and nursing home visits. Once a week, the inpatient care team holds the same IDT meeting, where colleagues who do work together every day pause to consider treatment options and suggestions.

By midmorning, visitors have begun to arrive. The front desk is staffed all day and evening, often by volunteers. They kindly greet each arriving party, explain the CT Hospice rules (especially during COVID), and comfort those waiting for a turn to go upstairs. Sometimes the lilting music of a grand piano drifts down the entrance hallway, where a volunteer plays for those who gather. It is not unusual to see a wheelchair or a bed rolled in for an impromptu or planned concert.
Those who work in support capacities are in full swing, paying bills, raising charitable funds to supplement Medicare reimbursements, hiring new staff members and volunteers, keeping track of all the rules and regulations that govern a hospice’s existence.

On nice days, families often take their loved ones outside. All the beds can be moved, and there is often a staff member or volunteer to help a patient who wants to be in the sunshine, but doesn’t have someone visiting. Small groups can be seen outside around the beds, at picnic tables scattered over the rolling lawn, or in the gazebo down by the double beach that gives the street its name. At high tide, that beach disappears, but, at low tide, family members can be spotted climbing on the rocks and enjoying the view. Raised flower beds grace the exit doors, reminding everyone of the circle of life.
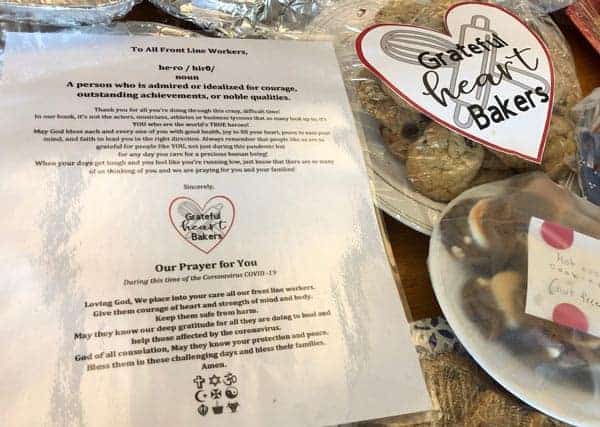
Lunchtime for patients happens as one would imagine, with trays delivered to beds. It’s not uncommon, however, to see a peach, some potato chips, or another treat sent up from the kitchen for a patient with a sudden craving. Some visitors bring favorite foods or drinks, while others (including staff), use delivery services from nearby restaurants. The staff eats on a separate floor, where the table is often piled with goodies brought by family members, or donated by outside groups. Halloween and Christmas both involve lots of extra calories!
All afternoon, there is a steady stream of ambulances delivering patients, or transporting respite patients back home. Each new arrival is greeted efficiently and compassionately. Those who enter in pain are usually made comfortable right away. By then, the evening shift has taken over, and new nurses and CNAs are checking on patient comfort levels, calling family members with updates, or attending to documentation on rolling computer trays.

Music and art therapists are going bed to bed, helping patients with requests or just easing loneliness. They have made videos for loved ones, collages, sketches, or other mementos. They help make Facetime calls to relatives, on iPads there for that purpose and play music that releases and relives old memories. Volunteers are also in full swing, either sitting quietly with those resting or wanting silence, chatting with others wishing for company, or playing music in the hallways. Some bring pets trained for visitation in hospitals, and they are particular favorites of everyone! Pastoral care professionals and volunteers visit each bedside, arrange for outside clergy when requested, pray with families, offer use of the prayer room tucked away down a side hall, or hold services in the common room.

As the sun sets, people pause to mark its beauty over the horizon, and begin winding down. Visitors still come, at all hours of the day and night, and the building is open around the clock. Cots are brought for those who plan to stay overnight. Clerical and support staffs head home, and the activity level goes down. People are still admitted during the off hours, but most are there, ready to be tucked in for the night.
And what of the patients in the beds? How does all of this activity affect them, in their final days? As many people have noted, at the end of life the days left are short, but the hours can be long. Decreased mobility, motivation, or purpose can diminish quality of life during a terminal illness. Volunteers, therapists, social workers, clergy, and medical staff all strive to help patients achieve closure, whatever that means for them, find peace, and eliminate pain and fear. To an astonishing extent, they succeed in that mission most of the time. Patients live fully until the end of their time, and find meaning and enjoyment wherever possible. As one patient famously said, “I came here to die, and I learned how to live.” They are the center of the hospice community, and they bask in that attention and concern.

Elsewhere in the facility, workers are still cleaning, cooking, fixing things, writing reports, and getting ready for the next day. Someone is always around, answering the phone for anxious family questions, dealing with crises in home care or in other settings, or completing yet another written report. Sometime during the night, someone changes the mat in the elevator to display the next day’s name (today is Wednesday), and another day begins, softly and lovingly.

As a not-for-profit, we depend on generous donors to help us provide customized services and therapies that aren’t completely covered by Medicaid, Medicare, or private insurance.
Please make a gift to help us sustain the highest standard of care.
Admissions may be scheduled seven days a week.
Call our Centralized Intake Department: (203) 315-7540.