Please view our updated COVID-19 guidelines and visiting procedures →.
Throughout the COVID-19 pandemic, the Medical Director at Connecticut Hospice, Dr. Joseph Sacco, has kept staff and volunteers well-informed of policy changes, PPE protocols, local and national COVID-19 data, and much more, through a “Daily Update” email.
He has also tested staff frequently for coronavirus to ensure a safe environment for all, and helped to care for non-COVID and COVID-positive patients alike, with his colleagues on the Interdisciplinary Team.
Some of the most appreciated and morale-boosting gestures he has shared with staff in his Daily Updates are the jokes and contests he has inserted at the end of each email.
A recent Haiku contest drew entries from almost every department of this non-profit organization - Nursing, Dietary, IT, Security/Building Services, Arts, Medicine, Social Work, Volunteers, Business office, & Administration. No subject was off-limits, although the COVID crisis was clearly on many minds. To read the entries, scroll below.
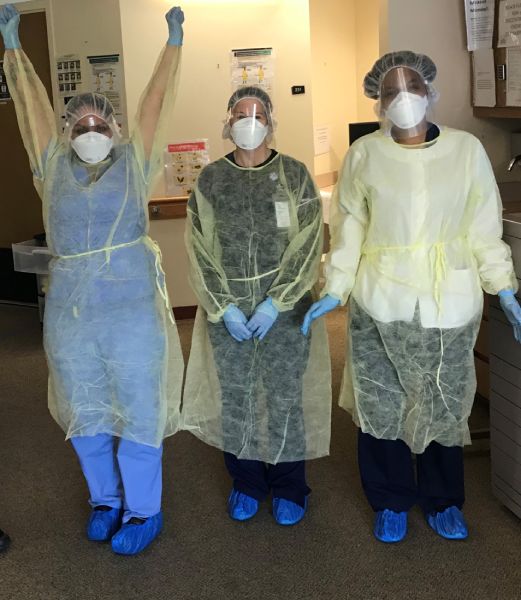
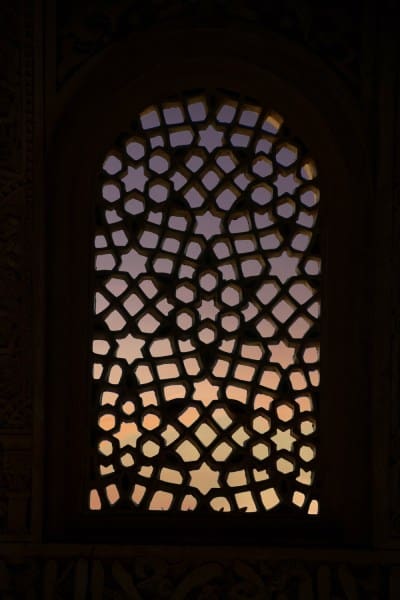
More recently, Dr. Sacco invited Connecticut Hospice staff to submit photographs on the theme “Beauty in Adversity”.
Window visits, at work and at home, were one recurring theme; social isolation featured prominently too. But love, family, humor and resilience were in strong evidence throughout.
We invite you to enjoy some of the submitted photographs, and may you find your own beauty in adversity.









Got both my gloves on
Ignoring my ear rug burn
Caused by my tight mask
Helping families
Supporting dying loved ones
Through their hardest times
I am leaving earth
Skies are calling me to go
My nurse lifts me up
My nurse blesses my
Last breath as I float away
No pain, only love
There was a big tree
That was in the blue ocean
We love that big tree
We will live to fight
That dreaded Covid nineteen
We will hug again
Our workers need masks
So who are you gonna call
Gonna call Batman
Dress in blue scrubs again
Think about some jewelry. Nah.
Lipstick on a pig.
Wash your hands, be safe
Put on a face mask people
Social distance now!
Patience takes hard work
Humans need much more practice
Smiling helps a lot
Gloomy rainy skies
Give way to sunny weather
I want summer heat
This too shall pass then
We will celebrate our work
Each other our caring
Can’t keep my mouth shut
The filter has big holes
Orange looks good on me
Another day home
Yet one more day staying home
Flattening the curve
Three days in the past
Or three days in the future
Fourteen days from then
alone a woman dies
fever ablaze yet pallid
breath halts then expires
Bud, breeze, buzz and bloom
Harken to our higher self
Faith in renewal
My feet in the sand
A frozen drink in my hand
Please bring on summer
In a world ablaze
We cry for our leaders help
The silence deafens
Touch my cheek softly
Say goodbye without weeping
Heaven awaits me
Fearsome pandemic
Exceptional caring folks
Clouds will part some day
Row, row, row our boat
Covidly down the stream, Life
Is NOT but a Dream
Homeschooling my kid(s).
Home care patients need me, too.
Remember to breathe.
Need toilet paper...
#askingforafriend
Charmin or Scott, Please?
Trip to London, nope
The high school musical, nope
First time to prom, nope
Zoom, zoom happy hour
One drink tastes good going down
Two, three even more
History and background of Haiku poetry
Using humor to cope with stress
How nature can restore your health
Ways to maintain your creativity and mental health
Have you seen Beauty in Adversity too? Capture what that means to you in a photograph and send it to us to share on this page. Do you love to compose haiku poetry? All photos and haikus must be your own work, must be copyright free, and you agree that there will be no financial liability to Connecticut Hospice or its employees if your entry is displayed.
Send photos and haikus to Director of Arts Katherine Blossom at [email protected]

When the COVID-19 pandemic forced millions into a form of hibernation, many found themselves existing in a much quieter world, some even experiencing long periods of silence. Some have found the opportunity to think and create in that unusually quiet space; others, (for most of us are social beings), have reached out on phones, FaceTime, and Zoom to feel a connection they have missed. Not everyone has that luxury, and many are painfully isolated – often the disempowered, the victimized, the poor, the sick.
Recently, regardless of the extent to which communities have lifted some social distancing restrictions, hundreds of thousands of citizens have been impelled to march en masse to protest violence and discrimination against people of color.
Whether in silence or in clamor, these sentinel events have emphasized the importance of listening to (and really hearing) others, and the importance of speaking up loudly for those who need support.

In this second installment of our series on Spiritual Care in Difficult Times, The Reverend Susan Trucksess, a Connecticut Hospice Pastoral Care Volunteer, examines the profound spiritual connection made when human beings sit in silence together, and the comfort and healing of solidarity, whether words are spoken or not.

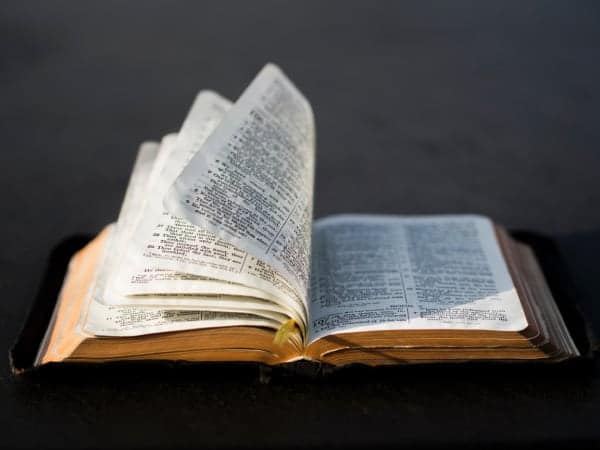
Presbyterians are wordy. Presbyterian ministers highly value the Bible as the Word of God, emphasizing Word. Presbyterian preachers preach long verbose sermons (Some might even say “endless.”) Presbyterian pastors use lots of words in conversations and communications with parishioners. (Some might even say “repetitive”). I am a Presbyterian minister...thus I tend to be wordy.
For many years I served in church settings. Then, in retirement, I came to Connecticut Hospice as a volunteer in the Pastoral Care department doing in-home care. I believed I had some experience to offer. Instead I learned I had much to learn... such as about the power of silence.
Naturally, in the course of my vocation, I had spent a lot of time with people in various straits of life, including but not exclusively those who were facing death. Now those at Connecticut Hospice who are moving toward the end of life in their homes are my “parishioners,” and our exchanges can have a different tone, a different quality, to them.



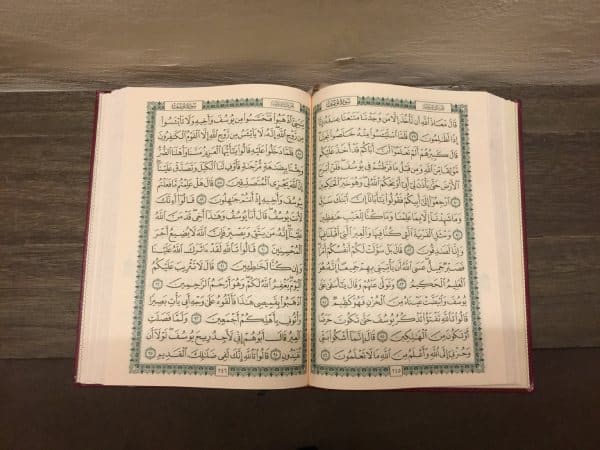
Often I walk into a home or a care center, sit at the bedside, and find that silence will be the most profound medium between the patient and me. Perhaps Mrs. Jones is presently too tired to talk. Maybe Mr. Gonzales has lost the ability to speak. Perhaps Rebecca is too angry or too sad to even look at me. John may be in a coma. What do I say in those situations? What words do I use? Of course, I can and do read from the Bible, the Torah, the Qur’an, if that seems appropriate or desirable. I can offer prayer, a blessing, an anointing, and spoken expressions of comfort and hope. And sometimes, sometimes, I can just sit in silence. As the Persian poet Rumi said,
"The quieter you become, the more you are able to hear".


At first, I have to admit, that seemed awkward. No words, no response. What was I doing there? What was I offering? Accomplishing? Nothing fancy, nothing bold, nothing noteworthy. It was humbling. And then I realized that was exactly the point, that is the point. In these moments I am sharing in the very human condition.
Each of us there - the patient and I - are going to die. Perhaps one sooner than the other, but each of us is living in the movement toward death. I am overwhelmed by a feeling of connectedness, of tenderness.
When two people (or more) know that we are in the process of being human, there is something that can happen between us. Something big, something grand, something tenderizing can take place in our midst. A kind of joy. All the things that normally distance us from one another become small and insignificant.
We will not be here forever, but we are here together now, and Spirit is with us. There can be joy in the midst of suffering, and life in the presence of death, as the wonder of life, death, and the mystery of life beyond death unfolds for all of us.

This is part of what Connecticut Hospice is all about - and it comes in many forms of caring for patients and families - with words, and without. It comes in a touch, a bandage, an injection, a bath, a warm meal, a smile, an assurance, a hope, a prayer. It comes from nurses and doctors, social workers, administrators, chaplains, aides, volunteers who cut hair, bring art supplies, music, (or dogs), transport to appointments. It comes through in-person interactions and in phone calls. It is soft and it is firm, compassionate and professional. It is caring and tending and accompanying. It is the Connecticut Hospice way. And we would be honored to serve you should you need us.
Peace and blessing, The Rev. Susan Trucksess, Pastoral Care Volunteer.
To read more on Presbyterianism: https://en.wikipedia.org/wiki/Presbyterianism
To find out more about 13th Century Persian poet Rumi's works: Rumi - America's best-selling poet
Rumi's life, death and legacy: Rumi biography
Writings on stillness: Stillness as action
Pablo Neruda on being quiet: Sylvia Boorstein reads Pablo Neruda poem
How U.S. Representative and civil rights leader John Lewis learned to use words for change: Excerpts from 'Preaching to the Chickens'

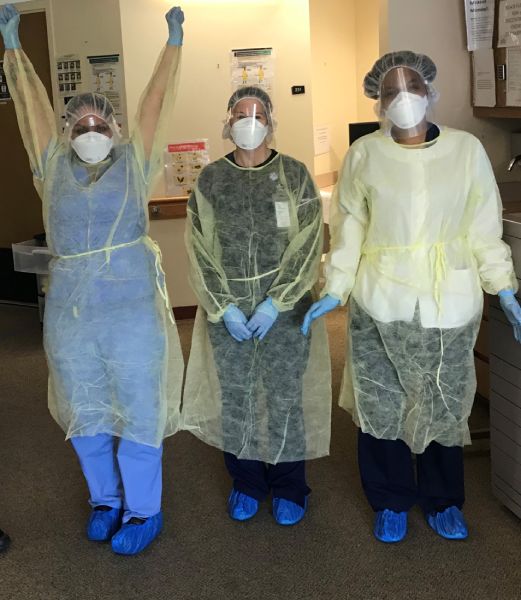
For all those isolated by illness and the pandemic, actress and Broadway star, five-time Tony Award nominee Laura Benanti has some joy to share, and we have been asked to help bring it to the Connecticut Hospice community and others who may not be active on social media and might be in need of connection during this time.
Benanti and social activist friend Kate Dieter-Maradei created SunshineConcerts, a free livestream concert series to connect an intergenerational audience.

This spring thousands of high school students across the country were bitterly disappointed to discover the musical productions they had spent months rehearsing would not be staged. On Twitter, Benanti invited students to share videos of the performances they weren’t able to give because of COVID-19.
The #SunshineSongs social media campaign went viral with millions of people joining the virtual audience for students’ heartwarming performances.
Benanti received thousands of videos from all over the country, (her friend Lin-Manuel Miranda watched many with her), and the story was featured on Good Morning America, Vogue, People and the NYTimes, etc,.
Benanti and Dieter-Maradei decided to turn this outpouring of expressions into something positive. The SunshineConcerts project livestreams performances by the best of the student submissions and includes performances by Laura Benanti, and other special guests so that elders and teenagers can come together in music.
Watch the The Sunshine Concert livestream Saturday, May 30 at 6pm! To make the event special, virtual tickets and playbills can be printed.
Download your SUNSHINEBILL Playbook here.
Download your Sunshine Concert ticket here.
Please share these details with anyone you know who is living in isolation during the Coronavirus Pandemic.

Pastoral Care is a core service of hospice care, an integral member of the interdisciplinary team that brings care to all hospice and palliative care patients and families. During difficult times, many seek solace in their spirituality, while others have many questions, and plenty of doubt, about where to find spiritual support.
It seems especially important to offer some reassurance while so many are struggling with current events. On this page we will be posting a series on how pastoral care providers at Connecticut Hospice see their mission, and how patients and families feel strengthened by their support, whether they follow a particular faith system or not.
In the first of this series, Jamie Johnson, Connecticut Hospice Pastoral Care Volunteer, defines how she sees Spiritual Care, and describes how it is given to hospice and palliative care patients in our in-patient setting and to patients at home throughout Connecticut.
Everyone has a worldview, a perspective on what is right or wrong, what is most important, what gives them comfort and inspiration, and why things happen. For many, their worldview is formed by their religion and faith communities. Others look to their human connections, to nature, to service, to love, something larger than themselves. This acknowledgement and embrace of something larger than ourselves, however you define it, is spirituality.
When crisis happens—unexpected change like losing a job, injury or illness, death—people turn to their sources of comfort and support, their spirituality, to make sense of what is happening. Some people pray to God, light a candle, meditate, take a walk outside, speak to a friend, clergy, or a therapist, create art. Sometimes, though, the crisis is so overwhelming they aren’t able to access that support. At Connecticut Hospice, this is where the chaplains and volunteers of the Pastoral Care department step in.
A sign in the Pastoral Care office reads:
Chaplains help create a sacred space for people of all faiths and cultural beliefs in stressful, life changing, or transitional moments to find meaning, hope, connection, and comfort by enabling them to identify and draw upon their inner strength.

This is spiritual care. Chaplains and volunteers offer their compassionate, calm, open presence to all people, from those in traditional faith communities to the “spiritual but not religious” and the “nones.” They will listen and provide support based on the careseeker’s beliefs.
Pastoral Careworkers do not preach or lecture; they do not judge or condemn. They sit at bedsides, hold hands, and hold space for people to process what troubles them; they may also offer prayer, ritual, or readings as appropriate.

If hospice patients or families need particular religious care, the department will contact local clergy. A prayer room is always available for prayer and meditation. Roman Catholic Mass is celebrated weekly, with communion available to those who can’t leave their rooms. Interfaith services are also performed regularly.
To support people of diverse beliefs, the Pastoral Care department works with the entire Connecticut Hospice team.

The Arts Department provides engaging and inspirational art projects and music at the bedside. Pet therapists bring dogs around for tender, loving care. Social workers listen and guide. There are special, handmade blankets on each bed to surround patients with color and warmth. Even our location on the shore of Long Island Sound offers a restorative breath of fresh air to patients and their loved ones.
The Pastoral Care department is here to help and support you during difficult and challenging times.
Jamie Johnson, Pastoral Care Volunteer, Connecticut Hospice

For information about different religions and spiritualities: Harvard Divinity School's Pluralism Project
For a series of inspiring podcasts on spiritual questions: Yale University's The Quadcast
To hear Yale University’s Shades of Yale perform uplifting spirituals: Amen & We Shall Overcome
To read A Prayer for Our Time, by The Rev. Frederick J. Streets, ’75 M.Div, Senior Pastor of Dixwell Congregational Church, New Haven, CT: A Prayer for Our Time
Resources on spiritual care and chaplaincy training:
Association of Clinical Pastoral Education
Association of Professional Chaplains
To learn more about Prayer Shawls and blessing blankets: Prayer shawl ministry
To donate new blankets to Connecticut Hospice, contact [email protected] or [email protected]

On a recent spring day, Sybil was brought down to the sunny lobby of Connecticut Hospice inpatient hospital in her bed. Social Work and Arts Department staff had collaborated over several days to orchestrate what was to happen when she got there. Her view through the floor-to-ceiling windows took in more than just the lawns stretching down to the sparkling water of Long Island Sound. On the other side of the glass, positioned six feet apart or more, were some of her closest family members. As staff music therapist Hannah Righter played “You’ll Never Walk Alone”, a favorite family song learned specially for this event, Sybil’s brother-in-law held up a large, colorful sign festooned with hearts, that read “Happy Anniversary”. Other family members held up phones to share this special day with a daughter in Tennessee. Her husband Don, sitting next to a vase of fresh tulips on a small table, leaned right up against the glass and spoke to her on a cellphone.
“It is so difficult not to be able to be with my wife now. Knowing I will see her through the window brings great joy”, he said before arriving. “I am very lucky to have such a wonderful family. I could not ask for more.”
As Hannah played “Five Foot Two, Eyes of Blue”, Sybil flashed a wide smile and sang along, tapping her hand.
This is how a couple who met days after Don’s return from service in the U.S. Army celebrate their 63rd wedding anniversary during coronavirus. When visiting guidelines are severely restricted by state executive orders, and parties must be made up of only a few, who cannot even hug each other, some have found a way to celebrate anyway.


Throughout the world, models of not only health care provision, but also basic human interaction, are being upended by the COVID-19 crisis.
How is hospice care adapting to this new landscape? How are patients and families continuing to receive the type of care and support which are the cornerstones of hospice care? In this article, we take a look at the ways in which Connecticut Hospice has adapted or transformed some of its programs both to meet patient and family needs, and to meet the challenges intrinsic to these times.
To enumerate the many changes and challenges, limitations and restrictions that have been placed on society in the past couple of months, and on health care providers in particular, is possibly redundant when the local and national news covers them almost exclusively on a daily basis. However, the ‘new normal’ presents specific challenges in a hospice setting, where one-on-one support, touch, unlimited family visiting, pet therapy, volunteers, bereavement support groups, and art and music therapies have been integral to hospice care for decades.
But hospice workers have always been resilient, resourceful and collaborative. Their work with patients and families has always required that they find alternatives, offer resources and solutions, empathy and understanding. This is especially true when one of the outcomes most wished for by the patients and families in their care – the cure of their incurable disease - is often beyond anyone’s capabilities.
So when infectious disease protocols and government executive orders limit close one-on-one contact with patients in the inpatient setting to certain staff, those staff-members must carry ever broader shoulders; they may be the only living beings patients can see for now and they must be almost all things to all people. The exception to this is when a patient nears the very end of life when hospice tenet dictates that no patient should die alone. Unlike the current policy in many hospitals, where COVID+ and other patients are not permitted visitors, at Connecticut Hospice, up to two family members may come at that time.
When patients cannot see facial expressions, now covered by masks and face shields, creative medical school students like Shayna Zanker step up to create large laminated badges featuring the friendly smiling face of each staff member.
Teamwork and professionalism under fire has allowed CT Hospice staff to pivot with agility, and to continue to offer excellent care and supportive programs to what is inarguably one of the most vulnerable populations.
The changes undertaken are not limited to emotional or psychological adaptations; technology is playing a huge role where physical contact is not possible. Social Work and Arts staff collaborate to facilitate 'virtual' visits using Facetime, Skype, Messenger, Zoom, etc. as well as taking people like Sybil to the lobby for family visits from the other side of the atrium windows.
Tele-Chaplaincy is now a staple of Pastoral Care. https://www.hospice.com/pastoral-and-spiritual-care/ Chaplains are praying with patients and families together on FaceTime. For Christians, communion is not held with tangible sacraments, but is spiritual and virtual. The advice that Reverend Warren Godbolt, Director of Pastoral Care, learned in theological school has taken on another layer of meaning these days –
“When you can’t find God’s hand, trust God’s heart”.
Bereavement support https://www.hospice.com/bereavement-program/ has been transformed by the COVID-19 pandemic as well. As in-person support groups were by necessity suspended, group members were contacted to inform them of on-line resources, including a Grief Group via Facebook by grief expert David Kessler. Group members are also encouraged to call the CT Hospice Bereavement Department for phone support any time. As on-line support is now being utilized much more during this time of social distancing, links to resources have also been added to the Bereavement page of the CT Hospice website and Connecticut Hospice Facebook page. Jennifer Stook, Bereavement Director, adds
“Every day we are learning new ways to connect to people needing grief or bereavement support and we are open to being creative while observing HIPAA regulations and privacy for those seeking assistance.”
Home care https://www.hospice.com/hospice-home-care/ staff have faced an array of challenges to their routines and work habits. PPE (personal protective equipment) is of course high on the priority list of caregivers who visit patients in homes and nursing homes, even in normal times. The extra layers of protection now required have to be changed, sanitized, or discarded, continually throughout the day. Some families desire to have no in-person visits in their homes currently at all, so ‘tele-health’ and careful communication and observation by phone or internet is a new option.
Home Care and Inpatient staff were already learning to navigate a range of new technologies connecting them with patients and each other throughout the past few years. The pandemic has accelerated that process. As Eric Smith, Information Systems Specialist, puts it:
“What was supposed to be a transition taking many months, became a transformation that has taken only a few weeks. We’ve taken a broad leap from a traditional information technology environment to one where we can provide and support patient-centered care anywhere, anytime, and on any type of device. We still have a way to go, but we are much, much further along in the process.”
Besides assisting patients and families to visit each other virtually, the Arts Program https://www.hospice.com/arts-program/ has digital exhibitions and music performances lined up to be broadcast on in-house bedside TV channels (for those without laptops or smartphones) until Arts staff and volunteers are permitted to return to making bedside visits.
The John D Thompson Hospice Institute, CT Hospice’s educational arm, https://www.hospice.com/jdt-hospice-institute/ hosts hundreds of interns and students in a normal year. Now, some of those students are finding helpful and creative ways to remain engaged. Students from Yale’s School of Organization and Management are hosting training courses for staff, and Medical and Nursing students are donning PPE and helping in both outpatient and inpatient settings.
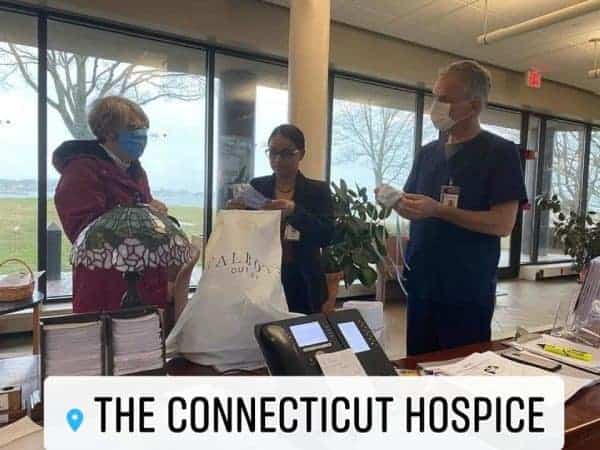
Perhaps the most moving example of the indomitable spirit of Hospice care has been the outpouring of generosity and involvement by CT Hospice Volunteers and the community at large. Early in the crisis, a Governor’s order suspended volunteer activities in hospitals. In Hospice care, volunteers serve in every discipline, and while they cannot now visit to help in person, this has not stopped them from remaining engaged on every level.
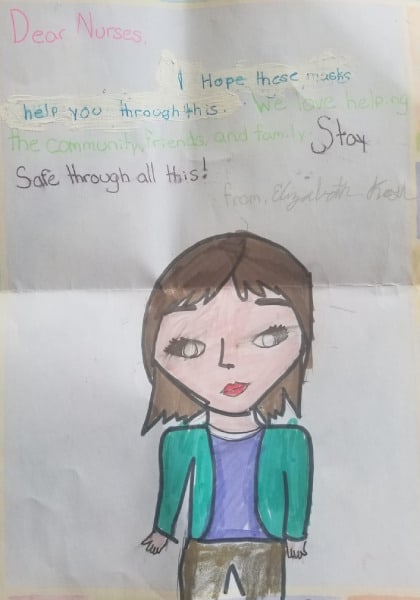

They have made hundreds of masks, sent music and messages on YouTube and Facebook videos, written articles, made phone calls, recruited donations of food and PPE. In the community, armies of furloughed workers are using sewing machines and 3-D printers to produce much-needed PPE, restaurants are donating meals, and everyone is banding together to help each other through the crisis.
The following has been making the rounds recently –
“FEAR has two meanings – Forget Everything And Run, or, Face Everything And Rise”.
The first option is not in the lexicon of hospice workers. Almost everything has changed in a few weeks. Almost. The mission and spirit of hospice care remain, stronger than ever.


For millions of people around the world a pandemic is a time of high anxiety and uncertainty, with reports indicating that stress levels of people isolated in their homes are higher than ever.
While perhaps more widespread now, this is not, however, a new phenomenon relating only to a pandemic.
For a person living with a life-shortening illness and receiving care at home, high anxiety and uncertainty, fear and exhaustion, are often already familiar burdens – not only for them but also for their family caregivers.
Each of us copes with tension, fear, and worry in different ways, and how your stress manifests itself physically, mentally and emotionally may dictate which strategies work best for you. Some find it easiest to unwind when their minds are engaged by something other than the source of their anxiety. Others feel more at peace when they’re getting things done, and some when they are doing nothing at all.
For many decades, the staff and volunteers of Connecticut Hospice https://www.hospice.com have observed how their patients and families cope best during these times, and have supported and empowered them to find their best strengths. There are almost as many strategies as there are individuals, but some common themes emerge which can be helpful to all of us, especially now.

If you are struggling with stress overload at home, consider some of the following strategies, which have proven effective for hospice and palliative care patients and families, individually and collectively, over many years.
Feeling overwhelmed can feel like being caught in a state of chaos, with no control over what happens. Empower yourself by putting some structure and routine into your life where you are able. Heighten your feeling of stability and control by setting the terms - block out time for certain tasks, choose a rhythm that works for you and your circumstances, repeat patterns that work.
A daily meditation coupled with yoga can help to center body and mind. Increased mental clarity can help to stabilize you. But you don’t have to practice formal meditation - simply concentrating your focus on one thing (a particular color, sound, word etc) can bring similar benefits.

If you have access to nature (even without being able to go out into the world at large), try focusing on transformation, growth, and rebirth by putting some energy into nurturing plant-life. Caring for living plants can give you deep satisfaction, and while ‘grounding’ yourself in this way, you have an opportunity to think about your worries more constructively. You may find peace and relaxation come more easily.
There is always someone somewhere who can and will help. It is not a weakness to need support. Very often others are grateful to have an opportunity to help you - it makes them feel good too.
https://www.hospice.com/pastoral-and-spiritual-care/
https://www.hospice.com/bereavement-program/
Gather as much real information as you can, without fixating on the source of your worries. Arming yourself with knowledge also empowers, and when you make decisions based on sound information, you are usually causing less additional stress down the road.

Keep things simple, do what you know you can and don’t feel guilt or anxiety if not perfect (see kindness to self!).
These don't only include structured games or traditional role-playing. Playful diversion can be healthy and relaxing (see kindness to self!)
When you think of an anxiety-provoking circumstance in your life, try to think of a positive aspect of it - (optimism!). Is there anything good that has come out of this?
Observe how your mind and body are handling stress.
Social interaction is vital to most human beings. Being a home-bound patient or caregiver can sometimes be lonely and isolating, but if you can share your feelings and experiences with others, even one other person, someone else is then helping to share your load (in a good way!). In-person conversations are usually most fulfilling, but if this is not possible, let technology be your friend. With so many options for communicating nowadays - phone, FaceTime, texting, messaging, Skype, social media such as FaceBook, Instagram, etc. on-line support groups and more – the rest of the world is not always far away. If you can, help a senior who may not have grown up using these media, to navigate them.

They often say that you cannot change circumstances or people outside yourself but you can learn to control your own responses and behaviors. This is easier said than done, of course. When you are exhausted, frightened, or angry this is especially hard. It takes discipline and energy that may be in short supply. One way to fuel up this positive energy is to perform an act of kindness (or think kindly and tolerantly of others) whenever you can. The rewards will last into your periods of lowest ebb. Don’t forget to be kind to yourself – jettison the idea that you must be perfect, treat yourself to a few minutes of time alone, pursue a favorite activity without guilt.
Experiencing pleasure in music lowers stress hormone levels, especially cortisol. Music can also cause activity in the nucleus accumbens and other reward areas of the brain that use the neurotransmitter dopamine, it can modulate activity in the amygdala, and it engages multiple brain regions involved in complex cognitive processing. These are all science-based ways of saying that music feels good, is relaxing and is often good for you.


Creativity is a life-force, and exploring your own can be exhilarating and rejuvenating, enlightening and empowering. Explore your imagination and creativity as inspiration and materials allow. Diverting your energy and focus from other worries in this way can be tremendously relaxing. Conversely, using an expressive medium to deliberately delve into the source of your stress can be profoundly illuminating. Processing and rendering something in your own way may render it no longer as threatening. Not only might you see something in a completely different way, but you might also see a new solution to a problem. https://www.hospice.com/arts-program/

Laughter is a well-known stress-reliever. Whatever makes you laugh, try to do some of it.

Get as much as you can, as regularly as you can, forsaking extra stimuli right before settling down. Keep your room dark and quiet through the night. Even short naps during the day can be restorative.

The garden’s grillwork gate
opens with the ease of a page
in a much thumbed book,
and once inside, our eyes
have no need to dwell on objects
already fixed and exact in memory.
Here habits and minds
and the private language
all families invent
are everyday things to me.
What necessity is there to speak
or pretend to be someone else?
The whole house knows me,
they’re aware of my worries and weakness.
This is the best that can happen –
what Heaven perhaps will grant us:
not to be wondered at or required to succeed
but simply to be let in
as part of an undeniable reality,
like stones of the road, like trees.
(translated from the Spanish
by Norman Thomas di Giovanni)


As a not-for-profit, we depend on generous donors to help us provide customized services and therapies that aren’t completely covered by Medicaid, Medicare, or private insurance.
Please make a gift to help us sustain the highest standard of care.
Admissions may be scheduled seven days a week.
Call our Centralized Intake Department: (203) 315-7540.