Please view our updated COVID-19 guidelines and visiting procedures →.

Connecticut Hospice community is fortunate to have many Pet Therapy Volunteers who bring their certified pet therapy dogs to visit our patients and families. While we can’t celebrate their special day in person because of the coronavirus, we want to honor them by sharing some of their pictures with you. Please enjoy these beautiful beings and join us in thanking them all!








Did you know there are other animal holidays? Here's a link to more special days for animals:https://www.dogtipper.com/fun/pet-holidays
For an article on the benefit of therapy dogs in hospice care, click here: The benefit of hospice therapy dogs
Resources for finding service dogs, therapy dogs, and other types of assistance dogs can be found here: Finding service, therapy & assistance dogs
This year has seen unprecedented challenges in every community. The health care community and the non-profit community each face tremendous demands, logistically and financially. Connecticut Hospice sits at the intersection of both communities, and we are consequently facing a year like no other.
We are grateful, therefore, to be among many Greater New Haven non-profit organizations who participate in The Great Give each year.
Entering its 11th year, The Great Give is an annual two-day online-giving event designed to support nonprofits throughout Greater New Haven County.
Due to COVID-19, the original 36-hour time frame of May 5th @ 8am through May 6th @ 8pm has been expanded: early giving is now open and giving will close on May 31st.
https://www.thegreatgive.org/organizations/the-connecticut-hospice-inc
Earn matching contributions from a $30,000 Griswold Home Care pool set aside for organizations that serve our elder community. Based on the number of unique donors Connecticut Hospice collects compared to just 11 other qualified organizations, a pro-rated amount will be awarded.

The Branford Community Foundation will award two prizes of $500 to Branford based organizations that receive donations from at least 30 unique donors prior to May 6th @ 8pm.


On a recent spring day, Sybil was brought down to the sunny lobby of Connecticut Hospice inpatient hospital in her bed. Social Work and Arts Department staff had collaborated over several days to orchestrate what was to happen when she got there. Her view through the floor-to-ceiling windows took in more than just the lawns stretching down to the sparkling water of Long Island Sound. On the other side of the glass, positioned six feet apart or more, were some of her closest family members. As staff music therapist Hannah Righter played “You’ll Never Walk Alone”, a favorite family song learned specially for this event, Sybil’s brother-in-law held up a large, colorful sign festooned with hearts, that read “Happy Anniversary”. Other family members held up phones to share this special day with a daughter in Tennessee. Her husband Don, sitting next to a vase of fresh tulips on a small table, leaned right up against the glass and spoke to her on a cellphone.
“It is so difficult not to be able to be with my wife now. Knowing I will see her through the window brings great joy”, he said before arriving. “I am very lucky to have such a wonderful family. I could not ask for more.”
As Hannah played “Five Foot Two, Eyes of Blue”, Sybil flashed a wide smile and sang along, tapping her hand.
This is how a couple who met days after Don’s return from service in the U.S. Army celebrate their 63rd wedding anniversary during coronavirus. When visiting guidelines are severely restricted by state executive orders, and parties must be made up of only a few, who cannot even hug each other, some have found a way to celebrate anyway.


Throughout the world, models of not only health care provision, but also basic human interaction, are being upended by the COVID-19 crisis.
How is hospice care adapting to this new landscape? How are patients and families continuing to receive the type of care and support which are the cornerstones of hospice care? In this article, we take a look at the ways in which Connecticut Hospice has adapted or transformed some of its programs both to meet patient and family needs, and to meet the challenges intrinsic to these times.
To enumerate the many changes and challenges, limitations and restrictions that have been placed on society in the past couple of months, and on health care providers in particular, is possibly redundant when the local and national news covers them almost exclusively on a daily basis. However, the ‘new normal’ presents specific challenges in a hospice setting, where one-on-one support, touch, unlimited family visiting, pet therapy, volunteers, bereavement support groups, and art and music therapies have been integral to hospice care for decades.
But hospice workers have always been resilient, resourceful and collaborative. Their work with patients and families has always required that they find alternatives, offer resources and solutions, empathy and understanding. This is especially true when one of the outcomes most wished for by the patients and families in their care – the cure of their incurable disease - is often beyond anyone’s capabilities.
So when infectious disease protocols and government executive orders limit close one-on-one contact with patients in the inpatient setting to certain staff, those staff-members must carry ever broader shoulders; they may be the only living beings patients can see for now and they must be almost all things to all people. The exception to this is when a patient nears the very end of life when hospice tenet dictates that no patient should die alone. Unlike the current policy in many hospitals, where COVID+ and other patients are not permitted visitors, at Connecticut Hospice, up to two family members may come at that time.
When patients cannot see facial expressions, now covered by masks and face shields, creative medical school students like Shayna Zanker step up to create large laminated badges featuring the friendly smiling face of each staff member.
Teamwork and professionalism under fire has allowed CT Hospice staff to pivot with agility, and to continue to offer excellent care and supportive programs to what is inarguably one of the most vulnerable populations.
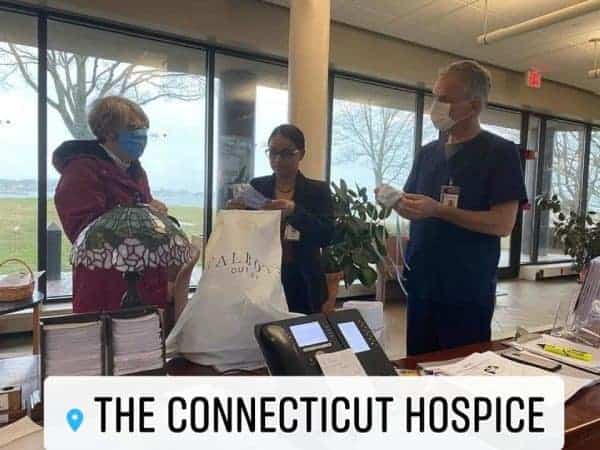
The changes undertaken are not limited to emotional or psychological adaptations; technology is playing a huge role where physical contact is not possible. Social Work and Arts staff collaborate to facilitate 'virtual' visits using Facetime, Skype, Messenger, Zoom, etc. as well as taking people like Sybil to the lobby for family visits from the other side of the atrium windows.
Tele-Chaplaincy is now a staple of Pastoral Care. https://www.hospice.com/pastoral-and-spiritual-care/ Chaplains are praying with patients and families together on FaceTime. For Christians, communion is not held with tangible sacraments, but is spiritual and virtual. The advice that Reverend Warren Godbolt, Director of Pastoral Care, learned in theological school has taken on another layer of meaning these days –
“When you can’t find God’s hand, trust God’s heart”.
Bereavement support https://www.hospice.com/bereavement-program/ has been transformed by the COVID-19 pandemic as well. As in-person support groups were by necessity suspended, group members were contacted to inform them of on-line resources, including a Grief Group via Facebook by grief expert David Kessler. Group members are also encouraged to call the CT Hospice Bereavement Department for phone support any time. As on-line support is now being utilized much more during this time of social distancing, links to resources have also been added to the Bereavement page of the CT Hospice website and Connecticut Hospice Facebook page. Jennifer Stook, Bereavement Director, adds
“Every day we are learning new ways to connect to people needing grief or bereavement support and we are open to being creative while observing HIPAA regulations and privacy for those seeking assistance.”
Home care https://www.hospice.com/hospice-home-care/ staff have faced an array of challenges to their routines and work habits. PPE (personal protective equipment) is of course high on the priority list of caregivers who visit patients in homes and nursing homes, even in normal times. The extra layers of protection now required have to be changed, sanitized, or discarded, continually throughout the day. Some families desire to have no in-person visits in their homes currently at all, so ‘tele-health’ and careful communication and observation by phone or internet is a new option.
Home Care and Inpatient staff were already learning to navigate a range of new technologies connecting them with patients and each other throughout the past few years. The pandemic has accelerated that process. As Eric Smith, Information Systems Specialist, puts it:
“What was supposed to be a transition taking many months, became a transformation that has taken only a few weeks. We’ve taken a broad leap from a traditional information technology environment to one where we can provide and support patient-centered care anywhere, anytime, and on any type of device. We still have a way to go, but we are much, much further along in the process.”
Besides assisting patients and families to visit each other virtually, the Arts Program https://www.hospice.com/arts-program/ has digital exhibitions and music performances lined up to be broadcast on in-house bedside TV channels (for those without laptops or smartphones) until Arts staff and volunteers are permitted to return to making bedside visits.
The John D Thompson Hospice Institute, CT Hospice’s educational arm, https://www.hospice.com/jdt-hospice-institute/ hosts hundreds of interns and students in a normal year. Now, some of those students are finding helpful and creative ways to remain engaged. Students from Yale’s School of Organization and Management are hosting training courses for staff, and Medical and Nursing students are donning PPE and helping in both outpatient and inpatient settings.
Perhaps the most moving example of the indomitable spirit of Hospice care has been the outpouring of generosity and involvement by CT Hospice Volunteers and the community at large. Early in the crisis, a Governor’s order suspended volunteer activities in hospitals. In Hospice care, volunteers serve in every discipline, and while they cannot now visit to help in person, this has not stopped them from remaining engaged on every level.
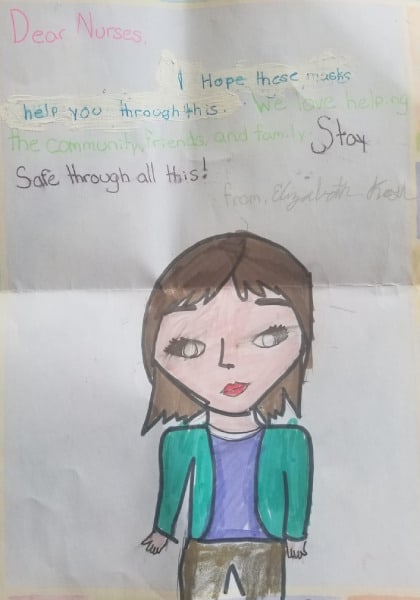

They have made hundreds of masks, sent music and messages on YouTube and Facebook videos, written articles, made phone calls, recruited donations of food and PPE. In the community, armies of furloughed workers are using sewing machines and 3-D printers to produce much-needed PPE, restaurants are donating meals, and everyone is banding together to help each other through the crisis.
The following has been making the rounds recently –
“FEAR has two meanings – Forget Everything And Run, or, Face Everything And Rise”.
The first option is not in the lexicon of hospice workers. Almost everything has changed in a few weeks. Almost. The mission and spirit of hospice care remain, stronger than ever.

Six members of the Yale Drama School costume shop staff have spent the past three weeks making some 400 cloth masks for donation to Connecticut Hospice.
“There had been so many conflicting messages about whether it would be a help to make masks,” mask-maker Pat Van Horn says. “To have Connecticut Hospice ask for them empowered me. I thought, ‘Okay, I know we are doing this for a reason.’ They will be used.”
Read the full article at https://news.yale.edu/2020/04/13/school-drama-mask-making-takes-new-meaning-and-urgency?utm_source=YaleToday&utm_medium=Email&utm_campaign=YT_YaleNews%20-%20Alumni%20From%20Peoplehub_4-15-2020

.
Read the full article at https://www.newhavenarts.org/arts-paper/articles/theater-artists-step-into-ppe-spotlight
As a not-for-profit, we depend on generous donors to help us provide customized services and therapies that aren’t completely covered by Medicaid, Medicare, or private insurance.
Please make a gift to help us sustain the highest standard of care.
Admissions may be scheduled seven days a week.
Call our Centralized Intake Department: (203) 315-7540.