Please view our updated COVID-19 guidelines and visiting procedures →.

On a recent spring day, Sybil was brought down to the sunny lobby of Connecticut Hospice inpatient hospital in her bed. Social Work and Arts Department staff had collaborated over several days to orchestrate what was to happen when she got there. Her view through the floor-to-ceiling windows took in more than just the lawns stretching down to the sparkling water of Long Island Sound. On the other side of the glass, positioned six feet apart or more, were some of her closest family members. As staff music therapist Hannah Righter played “You’ll Never Walk Alone”, a favorite family song learned specially for this event, Sybil’s brother-in-law held up a large, colorful sign festooned with hearts, that read “Happy Anniversary”. Other family members held up phones to share this special day with a daughter in Tennessee. Her husband Don, sitting next to a vase of fresh tulips on a small table, leaned right up against the glass and spoke to her on a cellphone.
“It is so difficult not to be able to be with my wife now. Knowing I will see her through the window brings great joy”, he said before arriving. “I am very lucky to have such a wonderful family. I could not ask for more.”
As Hannah played “Five Foot Two, Eyes of Blue”, Sybil flashed a wide smile and sang along, tapping her hand.
This is how a couple who met days after Don’s return from service in the U.S. Army celebrate their 63rd wedding anniversary during coronavirus. When visiting guidelines are severely restricted by state executive orders, and parties must be made up of only a few, who cannot even hug each other, some have found a way to celebrate anyway.


Throughout the world, models of not only health care provision, but also basic human interaction, are being upended by the COVID-19 crisis.
How is hospice care adapting to this new landscape? How are patients and families continuing to receive the type of care and support which are the cornerstones of hospice care? In this article, we take a look at the ways in which Connecticut Hospice has adapted or transformed some of its programs both to meet patient and family needs, and to meet the challenges intrinsic to these times.
To enumerate the many changes and challenges, limitations and restrictions that have been placed on society in the past couple of months, and on health care providers in particular, is possibly redundant when the local and national news covers them almost exclusively on a daily basis. However, the ‘new normal’ presents specific challenges in a hospice setting, where one-on-one support, touch, unlimited family visiting, pet therapy, volunteers, bereavement support groups, and art and music therapies have been integral to hospice care for decades.
But hospice workers have always been resilient, resourceful and collaborative. Their work with patients and families has always required that they find alternatives, offer resources and solutions, empathy and understanding. This is especially true when one of the outcomes most wished for by the patients and families in their care – the cure of their incurable disease - is often beyond anyone’s capabilities.
So when infectious disease protocols and government executive orders limit close one-on-one contact with patients in the inpatient setting to certain staff, those staff-members must carry ever broader shoulders; they may be the only living beings patients can see for now and they must be almost all things to all people. The exception to this is when a patient nears the very end of life when hospice tenet dictates that no patient should die alone. Unlike the current policy in many hospitals, where COVID+ and other patients are not permitted visitors, at Connecticut Hospice, up to two family members may come at that time.
When patients cannot see facial expressions, now covered by masks and face shields, creative medical school students like Shayna Zanker step up to create large laminated badges featuring the friendly smiling face of each staff member.
Teamwork and professionalism under fire has allowed CT Hospice staff to pivot with agility, and to continue to offer excellent care and supportive programs to what is inarguably one of the most vulnerable populations.
The changes undertaken are not limited to emotional or psychological adaptations; technology is playing a huge role where physical contact is not possible. Social Work and Arts staff collaborate to facilitate 'virtual' visits using Facetime, Skype, Messenger, Zoom, etc. as well as taking people like Sybil to the lobby for family visits from the other side of the atrium windows.
Tele-Chaplaincy is now a staple of Pastoral Care. https://www.hospice.com/pastoral-and-spiritual-care/ Chaplains are praying with patients and families together on FaceTime. For Christians, communion is not held with tangible sacraments, but is spiritual and virtual. The advice that Reverend Warren Godbolt, Director of Pastoral Care, learned in theological school has taken on another layer of meaning these days –
“When you can’t find God’s hand, trust God’s heart”.
Bereavement support https://www.hospice.com/bereavement-program/ has been transformed by the COVID-19 pandemic as well. As in-person support groups were by necessity suspended, group members were contacted to inform them of on-line resources, including a Grief Group via Facebook by grief expert David Kessler. Group members are also encouraged to call the CT Hospice Bereavement Department for phone support any time. As on-line support is now being utilized much more during this time of social distancing, links to resources have also been added to the Bereavement page of the CT Hospice website and Connecticut Hospice Facebook page. Jennifer Stook, Bereavement Director, adds
“Every day we are learning new ways to connect to people needing grief or bereavement support and we are open to being creative while observing HIPAA regulations and privacy for those seeking assistance.”
Home care https://www.hospice.com/hospice-home-care/ staff have faced an array of challenges to their routines and work habits. PPE (personal protective equipment) is of course high on the priority list of caregivers who visit patients in homes and nursing homes, even in normal times. The extra layers of protection now required have to be changed, sanitized, or discarded, continually throughout the day. Some families desire to have no in-person visits in their homes currently at all, so ‘tele-health’ and careful communication and observation by phone or internet is a new option.
Home Care and Inpatient staff were already learning to navigate a range of new technologies connecting them with patients and each other throughout the past few years. The pandemic has accelerated that process. As Eric Smith, Information Systems Specialist, puts it:
“What was supposed to be a transition taking many months, became a transformation that has taken only a few weeks. We’ve taken a broad leap from a traditional information technology environment to one where we can provide and support patient-centered care anywhere, anytime, and on any type of device. We still have a way to go, but we are much, much further along in the process.”
Besides assisting patients and families to visit each other virtually, the Arts Program https://www.hospice.com/arts-program/ has digital exhibitions and music performances lined up to be broadcast on in-house bedside TV channels (for those without laptops or smartphones) until Arts staff and volunteers are permitted to return to making bedside visits.
The John D Thompson Hospice Institute, CT Hospice’s educational arm, https://www.hospice.com/jdt-hospice-institute/ hosts hundreds of interns and students in a normal year. Now, some of those students are finding helpful and creative ways to remain engaged. Students from Yale’s School of Organization and Management are hosting training courses for staff, and Medical and Nursing students are donning PPE and helping in both outpatient and inpatient settings.
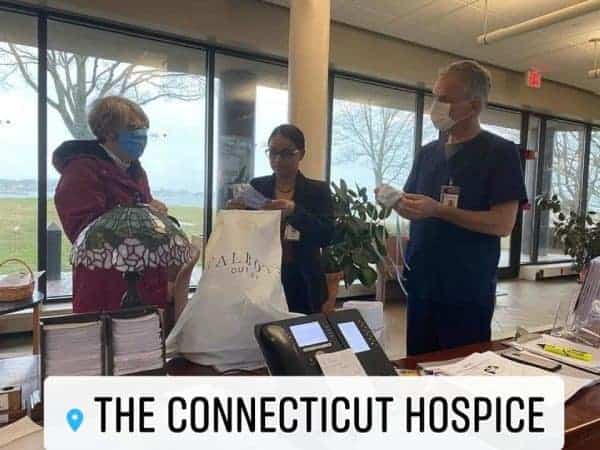
Perhaps the most moving example of the indomitable spirit of Hospice care has been the outpouring of generosity and involvement by CT Hospice Volunteers and the community at large. Early in the crisis, a Governor’s order suspended volunteer activities in hospitals. In Hospice care, volunteers serve in every discipline, and while they cannot now visit to help in person, this has not stopped them from remaining engaged on every level.
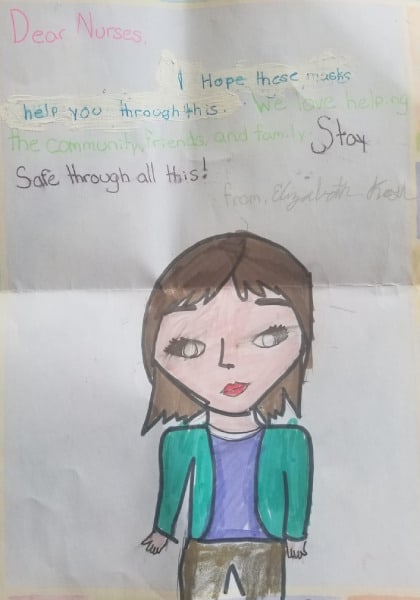

They have made hundreds of masks, sent music and messages on YouTube and Facebook videos, written articles, made phone calls, recruited donations of food and PPE. In the community, armies of furloughed workers are using sewing machines and 3-D printers to produce much-needed PPE, restaurants are donating meals, and everyone is banding together to help each other through the crisis.
The following has been making the rounds recently –
“FEAR has two meanings – Forget Everything And Run, or, Face Everything And Rise”.
The first option is not in the lexicon of hospice workers. Almost everything has changed in a few weeks. Almost. The mission and spirit of hospice care remain, stronger than ever.


For millions of people around the world a pandemic is a time of high anxiety and uncertainty, with reports indicating that stress levels of people isolated in their homes are higher than ever.
While perhaps more widespread now, this is not, however, a new phenomenon relating only to a pandemic.
For a person living with a life-shortening illness and receiving care at home, high anxiety and uncertainty, fear and exhaustion, are often already familiar burdens – not only for them but also for their family caregivers.
Each of us copes with tension, fear, and worry in different ways, and how your stress manifests itself physically, mentally and emotionally may dictate which strategies work best for you. Some find it easiest to unwind when their minds are engaged by something other than the source of their anxiety. Others feel more at peace when they’re getting things done, and some when they are doing nothing at all.
For many decades, the staff and volunteers of Connecticut Hospice https://www.hospice.com have observed how their patients and families cope best during these times, and have supported and empowered them to find their best strengths. There are almost as many strategies as there are individuals, but some common themes emerge which can be helpful to all of us, especially now.

If you are struggling with stress overload at home, consider some of the following strategies, which have proven effective for hospice and palliative care patients and families, individually and collectively, over many years.
Feeling overwhelmed can feel like being caught in a state of chaos, with no control over what happens. Empower yourself by putting some structure and routine into your life where you are able. Heighten your feeling of stability and control by setting the terms - block out time for certain tasks, choose a rhythm that works for you and your circumstances, repeat patterns that work.
A daily meditation coupled with yoga can help to center body and mind. Increased mental clarity can help to stabilize you. But you don’t have to practice formal meditation - simply concentrating your focus on one thing (a particular color, sound, word etc) can bring similar benefits.

If you have access to nature (even without being able to go out into the world at large), try focusing on transformation, growth, and rebirth by putting some energy into nurturing plant-life. Caring for living plants can give you deep satisfaction, and while ‘grounding’ yourself in this way, you have an opportunity to think about your worries more constructively. You may find peace and relaxation come more easily.
There is always someone somewhere who can and will help. It is not a weakness to need support. Very often others are grateful to have an opportunity to help you - it makes them feel good too.
https://www.hospice.com/pastoral-and-spiritual-care/
https://www.hospice.com/bereavement-program/
Gather as much real information as you can, without fixating on the source of your worries. Arming yourself with knowledge also empowers, and when you make decisions based on sound information, you are usually causing less additional stress down the road.

Keep things simple, do what you know you can and don’t feel guilt or anxiety if not perfect (see kindness to self!).
These don't only include structured games or traditional role-playing. Playful diversion can be healthy and relaxing (see kindness to self!)
When you think of an anxiety-provoking circumstance in your life, try to think of a positive aspect of it - (optimism!). Is there anything good that has come out of this?
Observe how your mind and body are handling stress.
Social interaction is vital to most human beings. Being a home-bound patient or caregiver can sometimes be lonely and isolating, but if you can share your feelings and experiences with others, even one other person, someone else is then helping to share your load (in a good way!). In-person conversations are usually most fulfilling, but if this is not possible, let technology be your friend. With so many options for communicating nowadays - phone, FaceTime, texting, messaging, Skype, social media such as FaceBook, Instagram, etc. on-line support groups and more – the rest of the world is not always far away. If you can, help a senior who may not have grown up using these media, to navigate them.

They often say that you cannot change circumstances or people outside yourself but you can learn to control your own responses and behaviors. This is easier said than done, of course. When you are exhausted, frightened, or angry this is especially hard. It takes discipline and energy that may be in short supply. One way to fuel up this positive energy is to perform an act of kindness (or think kindly and tolerantly of others) whenever you can. The rewards will last into your periods of lowest ebb. Don’t forget to be kind to yourself – jettison the idea that you must be perfect, treat yourself to a few minutes of time alone, pursue a favorite activity without guilt.
Experiencing pleasure in music lowers stress hormone levels, especially cortisol. Music can also cause activity in the nucleus accumbens and other reward areas of the brain that use the neurotransmitter dopamine, it can modulate activity in the amygdala, and it engages multiple brain regions involved in complex cognitive processing. These are all science-based ways of saying that music feels good, is relaxing and is often good for you.


Creativity is a life-force, and exploring your own can be exhilarating and rejuvenating, enlightening and empowering. Explore your imagination and creativity as inspiration and materials allow. Diverting your energy and focus from other worries in this way can be tremendously relaxing. Conversely, using an expressive medium to deliberately delve into the source of your stress can be profoundly illuminating. Processing and rendering something in your own way may render it no longer as threatening. Not only might you see something in a completely different way, but you might also see a new solution to a problem. https://www.hospice.com/arts-program/

Laughter is a well-known stress-reliever. Whatever makes you laugh, try to do some of it.

Get as much as you can, as regularly as you can, forsaking extra stimuli right before settling down. Keep your room dark and quiet through the night. Even short naps during the day can be restorative.

The garden’s grillwork gate
opens with the ease of a page
in a much thumbed book,
and once inside, our eyes
have no need to dwell on objects
already fixed and exact in memory.
Here habits and minds
and the private language
all families invent
are everyday things to me.
What necessity is there to speak
or pretend to be someone else?
The whole house knows me,
they’re aware of my worries and weakness.
This is the best that can happen –
what Heaven perhaps will grant us:
not to be wondered at or required to succeed
but simply to be let in
as part of an undeniable reality,
like stones of the road, like trees.
(translated from the Spanish
by Norman Thomas di Giovanni)


Every human being's life story is utterly unique - in the history of the planet nobody has ever shared your exact sequence and range of life experiences or ever will again. That makes your story, and every other human being's story, special and worth honoring.
When people share stories of their lives with others, they may remember and speak of details that are particularly meaningful to them, whether they are the essential milestones or the fleeting insignificances. Others who shared the original experiences may remember and speak of them divergently. Memory often works in this individualizing way
The work of the Arts Program of Connecticut Hospice draws forth abundant examples of this. Patients and their family members are offered a wide number of activities and therapies which, among many other things, encourage self-expression. Like narratives or aromas, it is well known that color and music are not only capable of evoking powerful emotions but are also redolent of deeply held memories. Many pages have been written on the power of music to help dementia patients, for instance, to connect with the past and relate to the present.
Whether interactions are during music therapy sessions, visual art activities, or any other modality, patients nearing the end of their lives almost universally engage in reminiscence or a form of life review.
At a point when most of their time on earth is behind them, patients inevitably draw on memory to communicate a sense of themselves. There is a need to take stock, to know that life has meant something, and that they have made, or are still making, their mark.
A more structured form of life review is practiced when patients actively discuss stages of life when prompted by specific questions and areas of focus. This is an important and widespread component of palliative and end of life care. Life Review at the end of life has the power to
Arts staff and volunteers at CT Hospice do not always deliberately guide a conversation in this way, but patients invariably share with Arts staff and volunteers their
Sometimes this is a spontaneous verbal conversation, sometimes it is recorded on video for family members to keep, and sometimes it may be represented in artwork or written word.
Amanda Salzano, ATR-LPC, staff art therapist, describes the aspect of legacy work she does with patients and family members as follows:
Art therapy offers opportunities for a patient to reflect upon his or her meaningful life experiences through art-making. The creative process transforms personal memories into tangible, visual representations that a patient can choose to share with others. For instance, a patient may choose to create personalized gifts to pass on his or her legacy and wisdom to family and friends, such as painting small rocks that represent life lessons and inspirational messages for others to carry with them after the patient has died.

Family members may not always be aware of every detail of their loved one’s life, but are usually very eager to honor and pay homage to them, and they enthusiastically join in sharing family stories at the bedside. Each patient and family member remembers something in their own way, making a patchwork quilt of memory, while the stories shared allow them to connect to the person they love before and after they are gone

New Haven-based artist Megan Craig has explored the themes of memory, connection and community, in her project “Memory Edit (I will never forget…)”, commissioned by Artspace for New Haven Citywide Open Studios in November 2019. This project explores the phenomenon of memory through touch, sound, and movement. The works consist of four fabric banners arranged with graphics and texts in hand-cut felt. Each banner represents memories from one of four artists in their 80s and 90s. During the weekend of Citywide Open Studios, sewing groups and individuals helped to hand stitch the felt onto the banners in a collective performance and sewing bee. These works will be exhibited at Connecticut Hospice in September & October of 2020.
"Memory Edit (I will never forget...) began with ideas about the precariousness of memory - how it slips over time. I hoped to create a work that makes memory tactile and invites people to collectively secure things in place. Sewing has a long history of being tied to memory communities and the production of objects and garments that safeguard memory. Stitching externalizes the internal process of committing something to memory, stitch by stitch, until it holds.

For this project I began by interviewing four individuals in their 80s and 90s. Each has led an extraordinary life of creativity. We talked about their earliest memories of making things (poems, dances, textiles, music, paintings, stage sets, buildings) and about their artistic lives. I annotated and edited the interviews to find dominant images and text. Later, I rendered those pieces in hand-cut felt and worked together with Nick Lloyd to create a sound tapestry of their voices.
In the studio I laid out a 6-yard train of fabric for each of the interviewees in a color that resonates with something in their story.
Gerry's banner is green; she told me she had red hair when she was young and always "looked smart in green". Alec's banner is blue for his earliest memory of crawling on the floor to trace the blue lines on a rug. Susan's banner is red for her cherry-colored pointe shoes. George's banner is the color of Louisiana Purple Pod Pole Beans.

Memory sits at the juncture of the individual and the collective. We have different memories of the same things. But memory is also built up over time, altered and adjusted, ripped and seamed. Memories, like fabric, can be vivid and whole or faded and threadbare. This work is about the possibilities for communal memory and the collaborative gesture of keeping memory intact."

For further reading:
THE BENEFITS OF REMINISCING
LIFE REVIEW THERAPY
LIFE REVIEW & QUALITY OF LIFE
CONNECTING GENERATIONS
ARTIST MEGAN CRAIG
ARTSPACE NEW HAVEN
CITY-WIDE OPEN STUDIOS

Caregiver burnout is a state of physical, emotional, and mental exhaustion from long-term stress and may be accompanied by a negative change in attitude and/or a loss of interest or motivation to care for a loved one.
Burnout can occur when caregivers don't get the help they need, and can affect caregivers’ emotional and physical health including symptoms such as fatigue, stress, anxiety, and depression.
On some days you may wonder what happened to your own life, your own health, and how you can continue to balance work and caregiving, let alone enjoy any social life or other activities.
You may see no end to the exhaustion and stress that caring for an elderly loved one can cause, however much you love them and want the best for them.
Many caregivers take on this role with little to no previous experience, and there are not always readily available support systems to help them.
The Bureau of Labor Statistics found recently that over 40.4 million American adults were unpaid caregivers of adults ages 65 or older, and this number grows every year.
Your Health: Under these circumstances, then, it is easy to imagine the devastating effects that can arise, most often manifesting in both emotional and physical stress and poor health.
Your Relationship: Sometimes caring for an aging and seriously ill loved one is not only physically and emotionally exhausting, but their relationship and communication with you can be irrevocably changed by this very illness. Do you remember when you didn’t talk with them about remembering to take medication or what the next steps in treatment might be, or how to handle their financial and legal issues, back when life seemed free of these approaching clouds?
Caregiver Burnout: In extreme cases, caregiver burnout and mental health issues like depression and anxiety can develop, along with emotions such as anger, guilt, resentment, and compassion burnout. Caregivers experiencing burnout often withdraw from friends and family, adopt abnormal eating and sleeping patterns, and catch more illnesses due to a compromised immune function. In extreme cases, their ability to care about the wellbeing of themselves or the recipient of their caregiving is reduced.

Even health care professionals need to be vigilant about self-care. If you are caring for a loved one, the emotional burden is usually greater still, and the need for self-care more urgent.
The Medicare Hospice Benefit covers up to five days of Respite Care for family members of hospice patients who are in need of a break from care-giving.

[The Bureau of Labor Statistics defines eldercare providers (here referred to as caregivers) as anyone of age 15 and older who has provided unpaid care to any adult age 65 and older in the last 3-4 months because of a condition related to aging. ]
Sources: [https://www.agingcare.com/articles/signs-of-caregiver-burnout]; [https://www.caregiver.org/caregiver-statistics-demographics]; [National Alliance for Caregiving and AARP. (2015). Caregiving in the U.S.]; [Institute on Aging. (2016). Read How IOA Views Aging in America
As a not-for-profit, we depend on generous donors to help us provide customized services and therapies that aren’t completely covered by Medicaid, Medicare, or private insurance.
Please make a gift to help us sustain the highest standard of care.
Admissions may be scheduled seven days a week.
Call our Centralized Intake Department: (203) 315-7540.