Please view our updated COVID-19 guidelines and visiting procedures →.

Having seen tens of thousands of patients over the past five decades, The Connecticut Hospice has the highest amount of professional skills for end-of-life care management. Over time, The Connecticut Hospice has progressed from its original beginnings—providing care for cancer patients and their families—into serving all patients, regardless of diagnosis. One of the conditions which has seen a huge increase in incidence is dementia, in part because other diseases can be cured or controlled, leaving more people to suffer from mental decline at the end of life. This can be particularly hard on families, who are often grieving the loss of the person they knew, while that loved one is still alive. Our new program, Magnolia Care, will increase the services and support to patients and families with Alzheimer’s disease, and other cognitive failures.
The training that we are giving to our nurses, aides, and social workers, combined with our longstanding knowledge of treatment options that preserve quality of life, has allowed us to design Magnolia Care in the most thoughtful of ways. In order to best understand what we are offering, it will help to provide some explanation of the progression of dementia.


Between 5 and 8% of the U.S. population over 65 is living with some form of dementia, with that number rising to 50% of those over 85. Dementia is defined as cognitive changes that affect thinking, personality, and behavior. It can be difficult to diagnose in its earlier stages and can be confused with other causes of those same symptoms. However, it occurs broadly across these age groups and is expected to increase as life expectancy rises and more people enter this demographic.
Early phases of the disease can often be managed by families without outside support. Minor adjustments in daily living arrangements, or additive monitoring of complex tasks, can suffice for some period of time. Independent living may be a challenge but is sometimes prolonged with enough support from relatives or paid caregivers.
The final stage of most diseases of dementia occurs between 3 and 6 years after a diagnosis is made. The progression of the disease does not follow a specific timeline and is different in each case.
This period of advanced symptoms may be months or years in length and could include a variable course of events which is unpredictable. Regardless of the type of dementia, there are some typical features that are often common at this time:
Magnolia Care is designed specifically for persons living with dementia at the end of life. Nurses, social workers, chaplains, nurse aides, art and music therapists, and volunteers all undergo intensive training and are certified in person-centered dementia care and non-pharmacological interventions.
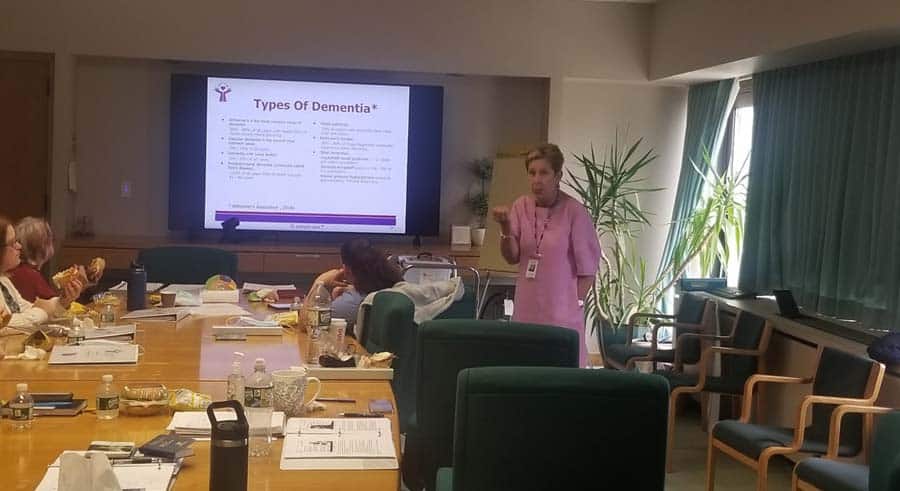
Our final-stage dementia care training was created by a hospice nurse with extensive experience caring for patients with dementia. This dementia-expert-lead training focuses on the behaviors and needs of hospice patients with cognitive failure, ensuring that Connecticut Hospice caregivers can recognize and respond to the concerns of dementia patients and families.
Like all of our Hospice Care programs, Magnolia Care provides a comprehensive approach that incorporates all the members of the hospice team in a plan of care that addresses the unique needs of each patient.
We have assembled a “tool kit” for use in homes, nursing homes, or assisted living, which offers enhanced tools for the management of symptoms, and can allow patients to access deeper memories, providing both solace and joy. The goals are to reach those patients where they are in their journey, help families to communicate and comfort their loved ones, and reduce the need for pharmacological solutions to common problems with behaviors.
Music is a known soother of dementia symptoms, and we work with caregivers to provide appropriate and significant music, tailored to the individual’s taste and age. MP3 players are embedded with this music in teddy bears, comfortably used by even people who are cognitively impaired.

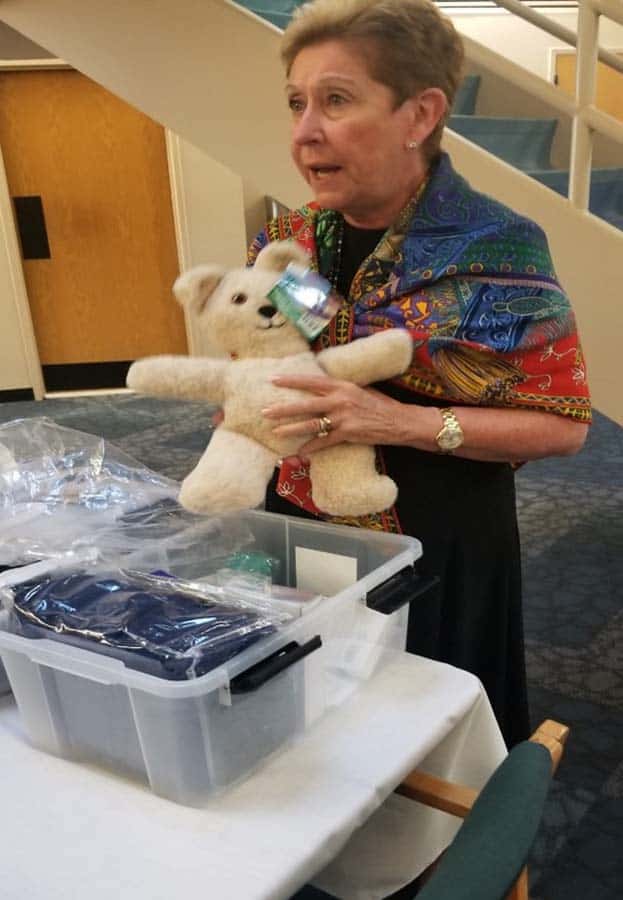
The toolkits also include a diverse range of items to help dementia patients and their caregivers, including:
These dementia care toolkits can be used by relatives, other caregivers, or those on the staff of busy skilled nursing facilities. These resources are packaged in a container made to fit by a bed or chair and is easily stored.
Finding a way to help those around the patient interact naturally and normally is critical in allowing the patient to retain function and, most importantly, dignity. Our staff’s training enhances skills required to meet the pressing physical and emotional needs of hospice dementia patients.

There is much more that can be written or read about cognitive decline at the end of life, but our goal here is merely to introduce some new concepts in dementia care, and to urge you to contact us if you or someone you love might benefit from Magnolia Care. It’s all part of what makes The Connecticut Hospice such a vital resource to both those we serve, and to the field as a whole.
As we close in on our fiftieth anniversary, we are trying, more than ever, to educate, serve, and advocate for those suffering from life-limiting illness. This is our latest milestone. We at The Connecticut Hospice are here to help.

As a not-for-profit, we depend on generous donors to help us provide customized services and therapies that aren’t completely covered by Medicaid, Medicare, or private insurance.
Please make a gift to help us sustain the highest standard of care.
Admissions may be scheduled seven days a week.
Call our Centralized Intake Department: (203) 315-7540.