Please view our updated COVID-19 guidelines and visiting procedures →.
As we approach the end of life, our bodies undergo various transformations, both internally and externally. One of the most noticeable changes can be observed in our skin. Understanding these skin changes is crucial for caregivers, medical professionals, and loved ones to provide appropriate care and support. In this comprehensive guide, we will explore the common skin changes that occur towards the end of life, their causes, implications, and strategies for managing them effectively. Any and all of these changes are considered a normal part of the natural dying process.

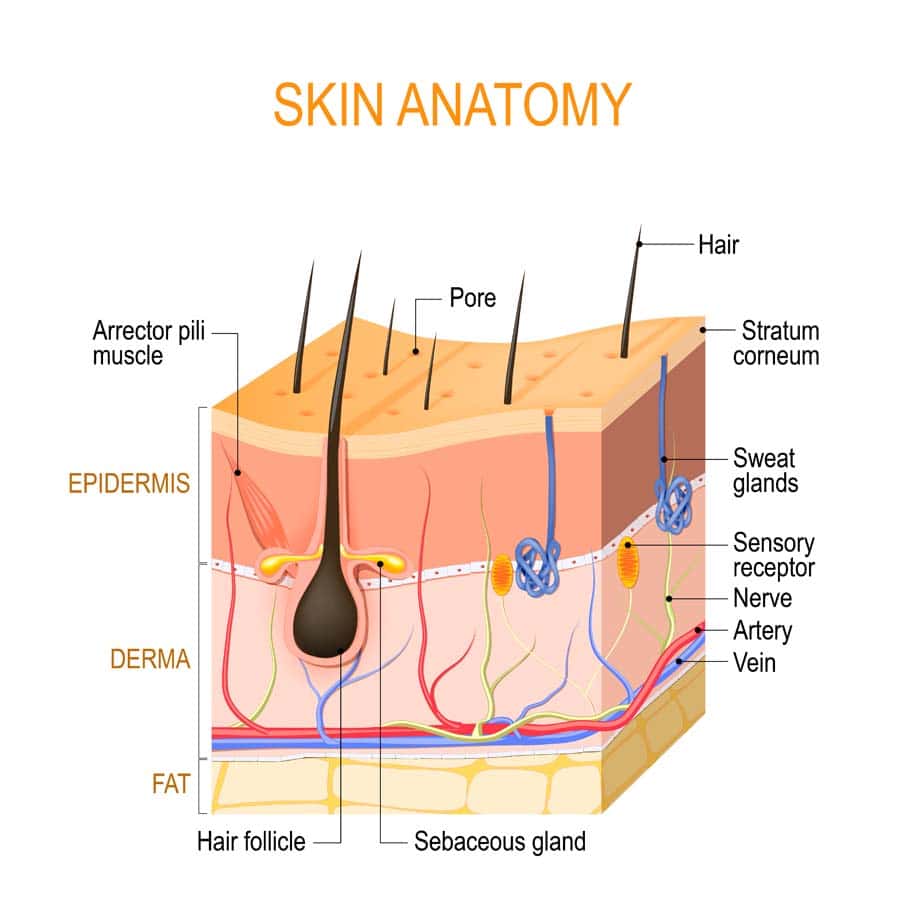
Circulatory Changes: Reduced blood flow to the skin contributes to pallor, mottling, and increased susceptibility to pressure ulcers. As the body's systems begin to shut down, blood is redirected to essential organs, leading to decreased perfusion of the skin and other peripheral tissues.
Dehydration: Diminished fluid intake or inability to process fluids properly can lead to dry, cracked skin. Dehydration is common in the end-of-life stage due to decreased oral intake, increased fluid losses, and metabolic changes.
Nutrition: Poor nutrition, common towards the end of life, can impair skin health and delay wound healing. Malnutrition, along with underlying medical conditions, can weaken the skin's structure and compromise its ability to withstand pressure and trauma.
Medications: Certain medications may affect skin integrity, moisture levels, and clotting mechanisms. For example, anticoagulants can increase the risk of bruising and bleeding, while diuretics may contribute to dehydration and electrolyte imbalances
Immobility: Limited mobility increases the risk of pressure ulcers and skin tears, as well as exacerbating circulation issues. Individuals who are bedridden or confined to a wheelchair are particularly susceptible to skin breakdown due to prolonged pressure and lack of movement.
Psychological and Emotional Impact of Skin Changes in Dying Patients
Skin changes can be distressing for both the individual nearing the end of life and their loved ones. Visible alterations in skin appearance may serve as a stark reminder of the person's declining health and mortality. Discomfort and pain associated with skin issues can also exacerbate emotional distress and affect overall well-being. It is important to discuss these changes with your medical provider and for the medical team to reassure and educate loved ones that these changes are a natural part of the dying process. Open and honest communication with the individual and their caregivers is essential to address concerns and provide reassurance. Emotional support, including validation of feelings and offering comfort, can help alleviate distress related to skin changes. Collaboration with healthcare professionals, including nurses, wound care specialists, and palliative care teams, is vital for comprehensive holistic care when it comes to managing these skin changes at end of life.

Providing dignified and comfortable care for individuals experiencing skin changes at the end of life is paramount. Respect for the individual's autonomy, privacy, and preferences should guide all aspects of care, including skin care routines and interventions. Encourage the individual or family members to participate in decisions regarding their care to promote a sense of control and agency.
Maintaining privacy and modesty is essential when addressing skin changes, as individuals may feel vulnerable or self-conscious about their appearance. Respectful communication and sensitivity to cultural and personal beliefs can help preserve the individual's dignity and promote a positive care experience. Additionally, incorporating rituals or practices that hold significance for the individual, such as religious ceremonies or personal grooming habits, can enhance their sense of well-being and spiritual comfort.

By understanding the causes and implications of these changes and implementing appropriate strategies, caregivers and loved ones can help maintain the individual's comfort and dignity during this challenging time. Through open communication and compassionate care, we can support those nearing the end of life in their journey with grace and dignity.
Understanding and addressing skin changes at end of life is essential for providing holistic care to individuals nearing the end of their journey. These changes, ranging from pallor and mottling to pressure ulcers and skin tears, are natural manifestations of the body's decline and require thoughtful management to maintain comfort and dignity. By recognizing the contributing factors, implementing appropriate interventions, and fostering open communication and support, caregivers, medical professionals, and loved ones can help alleviate distress and enhance quality of life for those in their care.
As we navigate the complexities of end-of-life care, it is crucial to uphold the principles of dignity, compassion, and respect for the individual's autonomy and preferences. Each person's journey is unique, and tailoring care approaches to meet their specific needs and wishes is paramount. Through this understanding, we can ensure that individuals facing skin changes at the end of life receive compassionate and comprehensive care that honors their humanity and affirms their inherent worth. Together, we can embrace the journey with empathy and grace, providing solace and support to those embarking on life's final chapter.

As a not-for-profit, we depend on generous donors to help us provide customized services and therapies that aren’t completely covered by Medicaid, Medicare, or private insurance.
Please make a gift to help us sustain the highest standard of care.
Admissions may be scheduled seven days a week.
Call our Centralized Intake Department: (203) 315-7540.